How High Blood Urea Nitrogen Increases Your Risk of Death with CKD
Why monitoring Blood Urea Nitrogen (BUN) could be the key to slowing CKD progression, protecting your heart, and living longer.
When you're diagnosed with chronic kidney disease (CKD), one of the first things your doctor might tell you is to reduce your protein intake. But why does this matter so much? The answer lies in a small but powerful substance called urea—specifically, Blood Urea Nitrogen (BUN).
What Is Urea and Why Does It Matter?
Urea is a substance produced by your liver when your body breaks down proteins. After it's created, urea enters your bloodstream and is filtered out by your kidneys, eventually leaving the body through urine.
But when your kidneys are not functioning properly, as in CKD, urea isn’t removed effectively. It starts to accumulate in the blood, which can lead to toxicity and contribute to complications—even increasing your risk of death.
That’s why monitoring BUN levels is such a critical part of managing CKD.
What the Urea Test Can Tell You
The urea test (BUN) provides important insights into your kidney and liver function, as well as your body’s ability to handle protein. Here’s what it can reveal:
1. Monitoring Disease Progression
In CKD stage 3, urea levels are significantly higher than in healthy individuals. For example, research shows salivary urea concentrations are about 6.8 ± 0.7 mM in people with CKD, compared to 4.1 ± 0.5 mM in healthy controls. This makes urea a useful marker for tracking disease progression.
2. Assessing Cardiovascular Risk
High BUN is not just a kidney concern—it’s a cardiovascular one too. Patients with the highest urea levels had a 93% higher risk of cardiovascular events compared to those with the lowest levels. That includes heart attacks and strokes.
3. Predicting Mortality
Studies have shown that people with elevated BUN levels have a higher risk of death even before reaching dialysis or transplant. It’s a strong indicator that the body is under metabolic stress.
4. Guiding Treatment Decisions
Urea, alongside creatinine, eGFR, and proteinuria, is among the top 10 markers used to predict how CKD will evolve. This helps nephrologists make better decisions about medication, diet, and timing for specialist care.
What High Urea Feels Like
Many people with CKD don’t notice when their urea is rising, but some common symptoms of high BUN include:
Persistent fatigue or weakness
Nausea or vomiting
Metallic taste in the mouth
Confusion or difficulty concentrating
Loss of appetite
Dry, itchy skin (uremic pruritus)
If you're experiencing any of these, ask your doctor about checking your BUN levels.
Diet and Urea: What You Eat Matters
Since urea is a byproduct of protein metabolism, your diet directly affects your BUN levels. Some tips:
Limit animal proteins, which tend to produce more urea than plant-based sources.
Choose low-protein alternatives like tofu, beans (in moderation for potassium), or lentils.
Avoid excess protein supplements, especially if they weren’t prescribed.
Work with a renal dietitian to find your personal protein target.
Hydration: A Simple but Powerful Strategy
Urea is excreted through urine—so if you're dehydrated, your BUN levels can rise even if your kidney function hasn't changed. Staying hydrated helps your kidneys do their job more effectively.
Tip: Unless your doctor has restricted fluids, aim for enough water to keep your urine light yellow. Dehydration can falsely raise BUN and stress your kidneys even further.
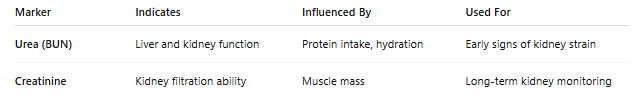
Urea vs. Creatinine: Know the Difference
Knowing both numbers gives a clearer picture of kidney health. Most doctors will test both together in a renal function panel.
How Often Should You Check BUN?
For people with CKD stage 3, BUN should typically be checked every 3–6 months, or more frequently if your condition is changing or you’re adjusting medications. Always ask your doctor what frequency is right for you.
Important Note: High BUN Doesn’t Always Mean Kidney Failure
BUN can be elevated for reasons other than kidney disease, including:
Dehydration
High-protein diet
Gastrointestinal bleeding
Certain medications
So don’t panic if your BUN is high—context matters, and your healthcare team will look at the full picture.
Can You Lower Urea Naturally?
Yes. Here’s how:
Eat less high-protein and processed food
Choose plant-based proteins over red meat
Stay hydrated
Avoid alcohol and unnecessary meds that stress the kidneys
Monitor portion sizes to reduce protein overload
These changes may seem small, but over time, they can make a real difference in your bloodwork—and your quality of life.
How the MetaSano App Helped Me — And How It Can Help You Too
The app uses my lab results, including urea levels, to recommend ingredients that are safer for my kidneys. That means I get personalized nutrition guidance tailored to my current health status.
One of my favorite features is how it helps me track my daily protein intake. Based on my weight, MetaSano automatically calculates my ideal protein limit. All I have to do is snap a photo of my plate — the app recognizes the ingredients and portion sizes, then tells me exactly how much protein I’m consuming. That way, I stay within my daily limits without having to guess.
It also shows me how well my meals adhere to my personalized diet, helping me stay accountable and consistent.
I can even log my daily water intake to make sure I’m hitting my hydration goals — another key factor for kidney health.
👉 Download the app now at metasano.com
It’s free for 7 days, and after that, it costs less than 10 cents a day.
Final Thoughts
Urea is more than just a lab value—it’s a warning sign, a tracker, and sometimes even a lifesaver. For people with CKD, understanding and monitoring BUN is a key step in protecting not just your kidneys, but your heart, your health, and your life.
If you’re living with CKD, make sure to ask your doctor about your urea levels, and what steps you can take to keep them in check.
You have more power than you think—especially when it comes to what’s in your blood.
Stay informed. Stay empowered.
—
Ewerton
Living with CKD